Top 20 Essential Terms for Emergency Department Medical Scribes
In the high-pressure environment of emergency medicine, scribes are expected to capture every second with flawless accuracy. That means more than fast typing — it requires deep fluency in medical shorthand, clinical terminology, and context-specific documentation. Emergency department (ED) scribes don’t just record data; they are frontline communicators who must decode abbreviations like “STEMI” or “GSW” in real time, cross-reference them with patient history, and document them correctly across EHR systems without error.
Whether you're aiming to become a medical scribe or hiring for your ED team, mastering the right language is non-negotiable. From cardiovascular acronyms to trauma-specific codes, understanding and applying these terms instantly can mean the difference between accurate patient care and critical error. This guide breaks down the 20 most essential emergency room terms, explores how they’re used in high-stakes situations, and shows how scribes are trained to navigate this landscape through our industry-leading certification.
Why Medical Terminology Matters in Emergency Settings
Every second counts in the emergency department. For scribes, mastering clinical language is not just about efficiency—it’s a critical skill tied to patient safety, legal accuracy, and the integrity of the medical record. Emergency physicians speak in fast-paced shorthand, and scribes must translate fragmented input into structured, billable, and defensible documentation. Mishearing or mistyping a single term like “STEMI” or “CVA” could result in wrong orders, delayed interventions, or insurance denial.
Speed, Accuracy, and Legal Clarity
Emergency documentation has a dual audience: treating physicians and legal systems. Medical scribes serve as real-time transcribers of assessments, procedures, and orders. If terminology is misunderstood or omitted, the implications ripple beyond clinical care—affecting billing compliance, malpractice risk, and interdepartmental communication. Speed must be matched with certainty. Terms like “N/V” (nausea/vomiting) or “LOC” (loss of consciousness) might seem routine, but context defines urgency. An ED scribe needs to know when a term signals a coding opportunity or a red flag.
Terminology Standardization for Documentation
Standardized language allows healthcare teams to work across shifts, specializations, and systems. Abbreviations and acronyms—while efficient—can become liabilities when used inconsistently. For example, “CP” might mean chest pain in one case and cerebral palsy in another. Scribes must rely on standardized glossaries provided by EHR systems, billing guidelines, or physician protocols. They are also expected to flag ambiguous or undefined terms and request clarification during dictation.
Moreover, scribes trained in standardized emergency terminology can reduce documentation variability, enhance communication between care teams, and ensure downstream coding is accurate for insurance and audits. In fast-paced trauma cases, where a physician may list terms out of order or switch between systems (e.g., Epic smart phrases and verbal dictation), a medically literate scribe prevents confusion by streamlining fragmented data into precise summaries. That’s not just helpful—it’s vital.
20 Must-Know Emergency Department Terms
In the emergency department, clarity isn’t optional—it’s critical. Scribes must know how to instantly interpret and record terminology that spans multiple specialties. The terms below are categorized by their most common usage context. Each one is used daily in ED workflows and directly affects treatment pathways, coding outcomes, and patient safety.
| Category | Term | Description |
|---|---|---|
| Cardiovascular | STEMI | ST-Elevation Myocardial Infarction; requires immediate cath lab and documentation of ECG, troponins, and treatment response. |
| PVC | Premature Ventricular Contraction; document frequency and symptoms if irregular. | |
| RVR | Rapid Ventricular Response in atrial fibrillation; note rate changes and medication effect. | |
| CHF | Congestive Heart Failure; include history, current symptoms, and diuretic response. | |
| Neurological | CVA | Cerebrovascular Accident; document NIHSS score, last known well, and treatment decision. |
| TIA | Transient Ischemic Attack; resolve in <24 hours, track timing and neurology consult. | |
| LOC | Loss of Consciousness; describe timeline, duration, and return to alertness. | |
| GCS | Glasgow Coma Scale; record exact eye, verbal, and motor scores. | |
| Trauma/Ortho | GSW | Gunshot Wound; include entry/exit sites, EMS report, and bleeding status. |
| Fx | Fracture; note bone, laterality, displacement, and splint/reduction details. | |
| MVC | Motor Vehicle Collision; capture injury mechanism, seatbelt use, and airbag deployment. | |
| C-collar | Cervical Collar; log application, neurological checks, and clearance notes. | |
| Respiratory/GI | SOB | Shortness of Breath; include onset, severity, triggers, and related findings. |
| N/V | Nausea/Vomiting; record frequency, emesis color, and treatment response. | |
| COPD | Chronic Obstructive Pulmonary Disease; document oxygen status, medications, and improvement. | |
| Hematemesis | Vomiting of blood; describe color, volume, and related GI history. | |
| General Vitals | BP | Blood Pressure; include baseline, abnormal values, and medication response. |
| HR | Heart Rate; chart tachycardia/bradycardia trends and procedural effects. | |
| SpO2 | Oxygen Saturation; document method, levels before/after oxygen administration. | |
| Temp | Temperature; note route (oral/rectal), fevers, hypothermia, and resolution. |
Documentation Shortcuts and Templates Used by Scribes
In emergency medicine, scribes are expected to document rapidly and accurately, even when the clinical flow is chaotic. To meet this demand, top-performing ED scribes use a toolkit of documentation enhancers: smart phrases, templates, macros, and voice-recognition integrations. These tools do more than save time—they ensure standardization, minimize errors, and support physician billing.
Smart Phrases, Macros, and Voice Recognition Tools
Smart phrases (e.g., “.chestpain”) trigger preloaded templates that include structured HPI questions, ROS entries, and exam defaults. Scribes must personalize every smart phrase in real time to reflect the patient’s specific case. These phrases are particularly useful for common presentations like abdominal pain, trauma, or shortness of breath.
Macros go further—they automate blocks of text, diagnoses, and orders. In systems like Epic, macros can include dynamic fields that pull vitals, lab values, or medication lists directly into the note. Scribes use them to reduce repetitive typing while preserving clinical accuracy. However, overreliance on macros can introduce risk if fields aren’t edited precisely to match the encounter.
Voice recognition (e.g., Dragon Medical One) allows providers to dictate narrative segments while scribes follow and format. The scribe’s role is to monitor for dictation errors, fill gaps, and confirm proper abbreviation expansion. In high-volume EDs, real-time dictation paired with templated macros can increase documentation speed by over 40%.
System-Specific Templates for Structured Notes
Each EHR system (Epic, Cerner, Meditech) has its own logic for templates. Most systems separate the note into HPI, ROS, PE, and MDM sections. Scribes are expected to navigate dropdowns, checkbox fields, and auto-populated labs to ensure every data point aligns.
Trauma templates often require specific fields for GCS scores, mechanism of injury, and procedures like intubation or chest tube insertion. In contrast, medical templates may emphasize chronic condition management, ROS completeness, and treatment response tracking.
The key is not to use templates passively. A well-trained scribe adjusts every field to match real-time physician behavior, eliminates default redundancies, and flags missing clinical information. The goal isn’t speed for its own sake—it’s creating a clean, reviewable, and billable chart that aligns with both physician intent and regulatory standards.
| Component | Description | Purpose/Impact |
|---|---|---|
| Smart Phrases | Short commands that trigger pre-built templates for common complaints (e.g., “.chestpain”) | Speeds up documentation while maintaining consistency |
| Macros | Automate entire note sections or insert dynamic fields (labs, vitals, meds) from the EHR | Reduces manual entry and supports data accuracy |
| Voice Recognition Tools | Tools like Dragon Medical One enable physicians to dictate while scribes format and monitor | Increases note speed and accuracy, especially in high-volume EDs |
| System-Specific Templates | EHR-defined note structures (HPI, ROS, PE, MDM) with dropdowns, checkboxes, and auto-filled data | Ensures regulatory compliance and complete clinical documentation |
| Template Personalization | Scribes must edit defaults, remove irrelevant fields, and tailor content to the specific patient encounter | Prevents errors, billing issues, and supports physician accuracy |
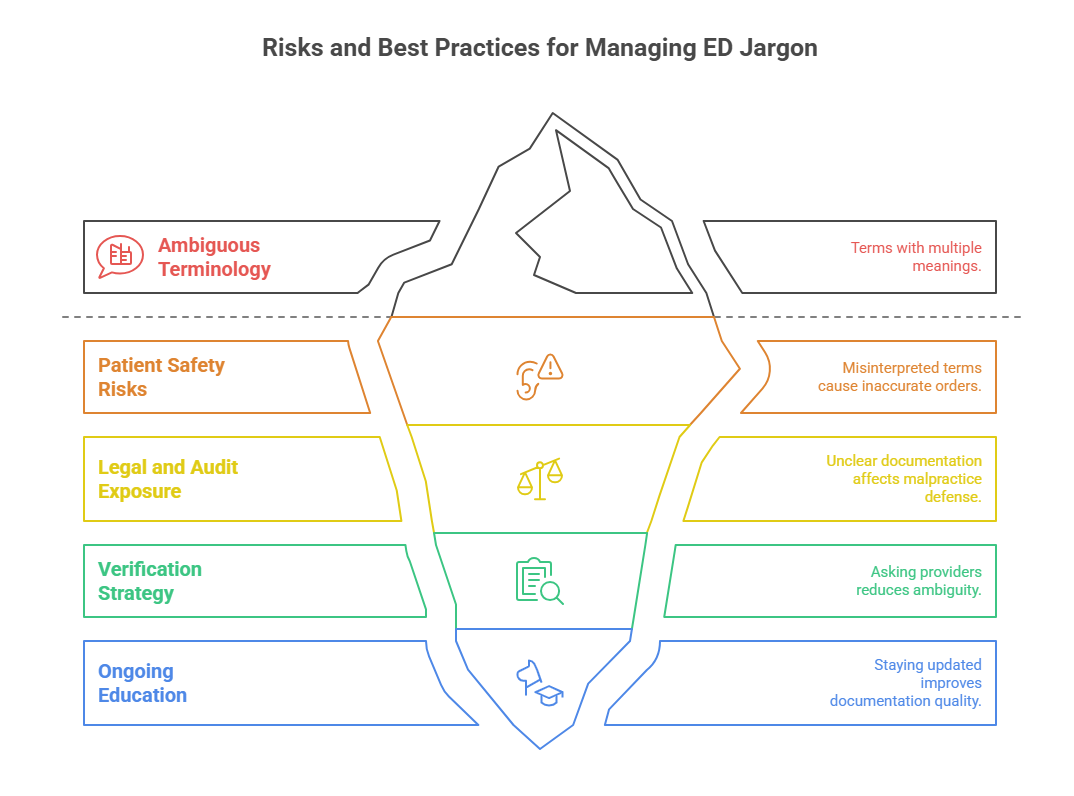
Risk of Misinterpretation: The High Stakes of ED Jargon
Emergency department communication thrives on shorthand—but when that shorthand is misunderstood, the consequences can be severe. Scribes working in EDs must balance speed with clarity, ensuring that every abbreviation they record reflects the exact clinical meaning intended by the provider. Misinterpretation doesn’t just slow down care—it can trigger legal claims, treatment errors, and dangerous delays.
Patient Safety and Legal Risks
Jargon in the ED is not standardized across all providers. “CP” might mean chest pain in cardiology but cerebral palsy in pediatrics. If a scribe documents an ambiguous term without clarification, it can lead to incorrect order sets, misfiled ICD codes, or even adverse patient outcomes.
For example, confusing “MS” (which may mean morphine sulfate or multiple sclerosis) can result in inappropriate medication administration or inaccurate history entries. From a legal standpoint, improper terminology affects malpractice defense, audit outcomes, and institutional liability. Notes with unclear abbreviations are frequently flagged during CMS audits, exposing hospitals to compliance penalties.
Scribes aren’t just typists—they’re clinical intermediaries responsible for capturing unfiltered physician intent in legally defensible language. That means being alert to terminology overlaps, spelling variations (e.g., “hematemesis” vs “hemoptysis”), and terms with multiple meanings in high-risk contexts.
Tips for Cross-checking Unfamiliar Abbreviations
Even experienced scribes encounter unfamiliar shorthand—especially in specialist consultations, trauma activations, or multi-system emergencies. Rather than guessing, elite scribes use structured strategies to verify terms before finalizing the chart.
Ask immediately if the term is critical or time-sensitive. It’s better to momentarily interrupt than submit an incorrect note.
Use embedded EHR glossaries, which provide institution-specific definitions and approved abbreviation lists.
Maintain a personal quick-reference sheet of high-risk or frequently misused terms encountered in prior shifts.
If the provider is unavailable, flag the section with a placeholder (e.g., “??”) and return to it before chart submission.
Regularly review terminology updates in EHR patches, especially after documentation template changes or software upgrades.
The goal isn’t to memorize every abbreviation—it’s to master the verification loop that prevents clinical ambiguity, coding misfires, and legal exposure.
How ED Scribes Improve Workflow Efficiency and Physician Focus
Emergency physicians face a relentless stream of patients, diagnostics, and split-second decisions. Without a scribe, providers spend up to 43% of their shift documenting—a major drag on both clinical focus and patient throughput. By integrating trained medical scribes into the care team, hospitals can reallocate that time toward diagnosis, procedures, and direct patient interaction.
Scribes reduce charting time by capturing notes in real time, pre-filling documentation templates, and prompting clarification for incomplete or vague physician statements. In a typical 8-hour shift, that translates into 90+ minutes of time saved per provider, which can enable higher patient volumes or improved consult depth.
From an operational perspective, ED scribes also help reduce charting backlog, minimize post-shift documentation, and improve coding accuracy through correct usage of terms like “Fx,” “RVR,” or “N/V.” As a result, hospitals report gains in provider satisfaction, reduced burnout, and more consistent reimbursement outcomes.
Ultimately, a well-trained scribe does more than transcribe—they optimize workflows. By mastering medical language, templates, and ED-specific systems, scribes help frontline physicians focus on what matters most: treating patients, not typing.
How Our Medical Scribe Certification Trains for ED Settings
Succeeding as an emergency department scribe requires more than textbook knowledge. You need immersive, real-world training that builds fluency in clinical shorthand, template-driven documentation, and rapid medical reasoning. Our program goes far beyond theory, equipping scribes to handle real ED workflows from day one.
The ACMSO Medical Scribe Certification Program is designed specifically for high-pressure environments like trauma bays, cardiac zones, and fast-track units. You’ll train in recognizing key emergency terms like STEMI, CVA, LOC, and SOB, while also learning how to apply documentation shortcuts, legal protocols, and EHR systems used in hospitals across the U.S.
What sets this program apart is its simulation-based training and case study-driven modules. You won’t just memorize abbreviations—you’ll apply them in time-sensitive scenarios, paired with mock dictations and physician-style narration. By the time you complete the certification, you’ll be prepared to create fully billable charts, support physician accuracy, and contribute to patient safety without hesitation.
If you’re ready to build mastery in fast-paced clinical documentation, explore the ACMSO Medical Scribe Certification Program and start your ED scribe journey with professional confidence.
Frequently Asked Questions
-
You don’t need a medical degree to become a scribe, but you do need strong knowledge of medical terminology, EHR systems, and fast, accurate typing skills. Most employers prefer candidates who’ve completed a certified scribe training program, especially one focused on emergency medicine. The ACMSO Medical Scribe Certification is highly respected in the field for its practical approach to ED-specific workflows. It prepares you for real-time documentation under pressure, legal charting standards, and advanced terminology used across trauma, cardiac, and neuro units. Prior experience isn’t required, but a background in biology or health sciences can be helpful.
-
Terminology mastery is essential because every second counts in the emergency department. An incorrect abbreviation or missed nuance can cause treatment delays, billing errors, or legal liability. For example, “CP” could mean either chest pain or cerebral palsy, depending on the context. Scribes must be able to decode acronyms like “STEMI,” “CVA,” and “N/V” instantly, then document them accurately. This ensures the chart reflects the physician’s intent and supports downstream teams like radiology, coding, and billing. Mastery also enables scribes to document more efficiently, reducing rework and helping providers move through patients faster.
-
A medical scribe in the ED should know at least 20 foundational terms, including STEMI (heart attack), CVA (stroke), LOC (loss of consciousness), SOB (shortness of breath), and Fx (fracture). These terms span across cardiovascular, neurological, trauma, GI, and vitals categories. Accurate usage impacts not just documentation, but also coding and continuity of care. Most of these abbreviations are used multiple times per shift, and many have legal or clinical implications if misused. A high-quality certification like the ACMSO Medical Scribe Certification Program provides practical training in applying these terms under live dictation pressure.
-
ED scribes rely on a mix of smart phrases, macros, voice-recognition software, and structured templates to keep pace with providers. These tools allow for rapid insertion of common terms and ensure charts remain consistent across providers. Scribes must learn to personalize templates during the encounter, adjust for clinical nuance, and flag anything ambiguous. In fast-paced settings like trauma bays or cardiac rooms, scribes may also use shorthand or placeholders and complete full entries immediately after the encounter. Training in systems like Epic or Cerner is also critical, since EHR navigation can make or break charting speed.
-
Misinterpreting medical jargon can lead to serious clinical and legal consequences. A common example is confusing “MS” for morphine sulfate versus multiple sclerosis, which could result in dangerous medication administration or inaccurate patient history. Incorrectly recording “RVR” or “GCS” can change triage level or delay specialty consults. From a legal standpoint, ambiguous notes weaken malpractice defense and can flag the chart during audits. Scribes are responsible for ensuring all terminology is accurate and context-specific. That’s why advanced training programs like ACMSO’s scribe certification teach both medical language and the verification protocols to prevent these risks.
-
The best approach is immediate clarification. If a provider uses an unfamiliar abbreviation, ask them directly—especially if it affects clinical accuracy, diagnosis, or legal defensibility. If they’re unavailable, insert a placeholder like “??” and highlight it for follow-up. Many EHR systems also have built-in glossaries or approved abbreviation lists to consult. Creating a personal cheat sheet of high-risk or department-specific terms can also help. Never guess or assume—it’s better to pause briefly than enter incorrect information. The ACMSO certification course includes a checklist of ambiguous terms and teaches techniques to verify meaning on the spot.
-
Voice recognition software like Dragon Medical One allows providers to dictate directly into the EHR. Scribes use these tools to capture narrative portions, such as history, physical exams, and medical decision-making. However, transcription isn’t automatic. Scribes must actively monitor for dictation errors, ensure proper formatting, and expand abbreviations accurately. For example, if a physician says “patient with SOB and CP,” the scribe must correctly interpret this as shortness of breath and chest pain, not copy the raw abbreviations. Training includes listening comprehension, formatting fluency, and editing for billing compliance—especially in high-speed ED environments.
-
Look for programs that combine terminology mastery, real-world EHR training, and ED-specific scenarios. Simulation-based modules, live dictation practice, and case-based learning are crucial. A top-tier program will also prepare you for legal documentation protocols, HIPAA standards, and physician communication techniques. The ACMSO Medical Scribe Certification covers all these elements with an emergency medicine focus. It includes over 170 hours of training, scenario walkthroughs, and a final assessment that mimics live ED conditions. If you want to hit the ground running in trauma bays, acute care, or fast-track units, this type of training is essential.
Final Thoughts
In the emergency department, there’s no margin for error. Medical scribes must work with precision, speed, and deep clinical awareness—especially when lives are on the line. Mastery of abbreviations, documentation templates, and terminology shortcuts isn’t optional—it’s the core of your role. Whether you're working behind the trauma curtain or tracking a stroke alert in real time, your ability to document with clarity directly supports patient outcomes, billing integrity, and legal safety.
If you’re serious about building this critical skill set, don’t settle for generic training. The ACMSO Medical Scribe Certification Program is designed for the realities of emergency care, giving you the tools to thrive on shift one. With hands-on training in EHR navigation, terminology drills, live simulations, and legal documentation strategy, it delivers career-ready preparation that hospitals trust. Become the scribe every ED physician wants by mastering the language that drives medicine forward—fast, accurate, and accountabe.
Poll: Which skill do you think is most essential for emergency department scribes?